Abstract
Background
The incidence, manifestations and risk of cerebrovascular disease (CVD) are not well known in recipients of allogeneic hematopoietic stem cell transplantation (HSCT). CVD, including ischemic or hemorrhagic stroke and posterior reversible encephalopathy syndrome (PRES), are important and potentially life-threatening post-transplant complications. Notably, there are few supporting results to explore these complications. We therefore aim to investigate the incidence, risk factors, and survival of post-transplant CVD.
Patients and Methods
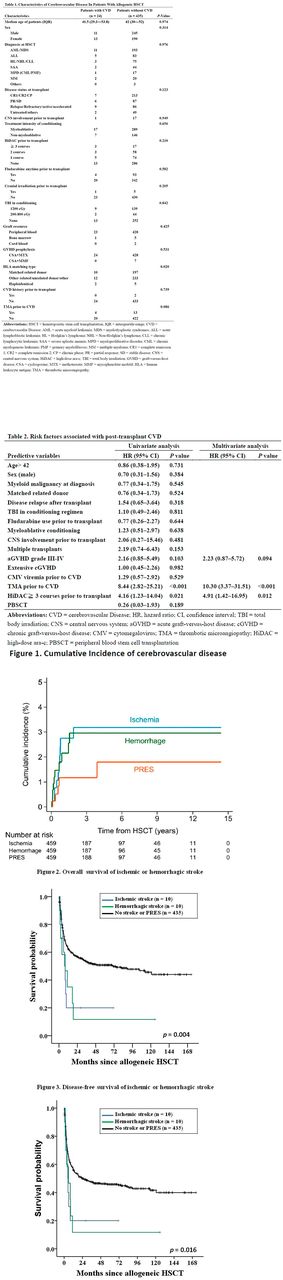
We included in this study 459 adult patients undergoing allogeneic HSCT at an Asian tertiary medical center between January 2003 and December 2015. A total 24 patients documented post-transplant ischemic or hemorrhagic stroke and PRES according to clinical neurologic signs and brain MRI. Clinical features, cumulative incidence, risk factors and survival for post-transplant CVD in recipients of HSCT were collected and analyzed.
Results
Post-transplant CVD occurred in 24 (5.2%) of 459 HSCT patients. One patient suffered from PRES initially, and subsequent ischemic stroke two months later. The cumulative incidences at days 100, one year and two years were 0.8%, 2.8% and 3.2% in ischemic stroke (n = 10), and 1.2%, 2.2% and 3.0% in hemorrhagic stroke (n = 10), respectively. In addition, the cumulative incidences of PRES (n = 5) at days 100, one year and two years were 0.2%, 1.2% and 1.2%, respectively. In the multivariate analysis, thrombotic microangiopathy (TMA) prior to CVD (adjusted hazard ratio [HR] 10.30, 95% confidence interval [CI]: 3.37-31.51) and high-dose ara-c (HiDAC) ≥ 3 courses prior to transplant (adjusted HR 4.91, 95% CI: 1.42-16.95) were identified as independent risk factors of post-transplant CVD. There was a trend as a risk factor in patients with grade III-IV acute GVHD (P= 0.094). For patients with post-transplant stroke, there were significantly lower disease-free survival (P= 0.016) and overall survival (P= 0.004).
Conclusion
The occurrence of CVD, especially for ischemic or hemorrhagic stroke after allogeneic HSCT, was associated with reduced survival. Identifying patients at risk, monitoring, early detection, and management of post-transplant CVD play roles to improve outcome. Patients with TMA prior to CVD and treatment of more than three HiDAC courses prior to transplant are at risk of CVD. Once a high-risk group is identified, much effort is required to target new approaches for prevention, early detection and treatment of this complication.
.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal